Running, at its basis, is about load tolerance. Refer back to the blog post on the envelope of function for more on this. Running injuries can be biomechanically explained by the idea that the load to an area exceeds its capacity for loading. At this point, we have a few options to intervene biomechanically. Physiotherapist (he’s Australian) Christian Barton has a nicely laid out guideline to organize these interventions called RISK:
R – reduce overall load
I – improve load capacity
S – shift the load
K – keep adapting to the runner’s goals/capacity
For part one of this blog post we’re going to talk about the R and S of RISK – reducing and shifting load. Before we can get to this, though, we need to know how the runner has been loading. In this instance I don’t mean studying their training plan, which we should also do (goes along with reducing overall load), I mean performing a clinical gait analysis.
Why gait analysis? Doesn’t everyone run the exact same and put the same amount of load into their joints? Short answer – no. Long answer – no, that’s not even close to realistic. Everyone runs differently and what works for some doesn’t work for others, but we can change some loading parameters if our goal is to optimize efficiency or shift load from one area to another (which should be used with caution). It’s not about vilifying movement, it’s about introducing variability into the system.
So, gait analysis. Subjectively analyzing movement. Sounds like that could be an issue if we can’t come to an agreement on what’s “normal”, right? As with most qualitative analyses, the things that are really noticeable are usually agreeable between testers, as per a reliability study by Pipken et al. in 2016. Unsurprisingly, the small variable/hard to notice things were not very well agreed upon. Anyway, we’ve got our runner on a treadmill running and we watch how they run from the side (sagittal plane) and from the back (frontal plane). Let’s assume this is the best and most realistic way to analyze how they run and see if they could benefit from changing anything (large assumptions). Here’s what we’re most focused on with some quick points:
Sagittal plane
- Step length / distance from initial contact to center of mass – while there aren’t normative values for this, this one is closely tied to cadence. Landing far in front of the center of mass puts the breaks on, it’s not efficient. We know that this can also contribute to increasing impact loading variables, whether or not it’s strongly tied to injury rate.

https://mensrunninguk.co.uk/wp-content/uploads/2016/06/overstride.jpg - Vertical oscillation – also tied to cadence, bounding higher with each step increases impact loading.
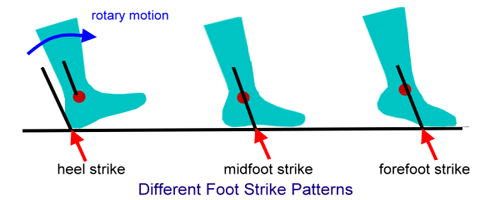
http://fellrnr.com/mediawiki/images/thumb/5/5b/Vertical_Oscillation.png/500px-Vertical_Oscillation.png - Foot strike pattern – there’s too much to dive into here but don’t worry, there will be a full blog post about this in the future. What I will BRIEFLY say is that we can change this temporarily to shift the load.
Frontal plane
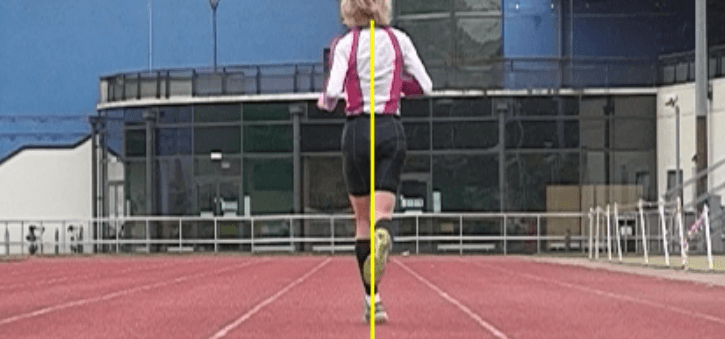
- Pelvic drop/knee window- potential to affect trunk lean, step width, and valgus position at the knee. Can be a factor to consider with hip, knee, and IT band pain.
https://encrypted-tbn0.gstatic.com/images?q=tbn:ANd9GcT8jcClgyGloDVCsfExPmwuLz2G8zZlLDDGF7grmYA0EfPxecz0 - Step width – again, no normative values but appears to have a relationship with IT band pain with crossover gait/very narrow step width.
https://www.kinetic-revolution.com/wp-content/uploads/2013/12/Screen-Shot-2013-12-15-at-21.09.37.png - Subtalar eversion or “pronation” – there’s not actually very much evidence to say this is an issue, nor is it something we can change with a cue…
Additional considerations
- Cadence – see previous blog post
- Sound upon impact – see cadence post, also an indication that our runner is hitting hard and taking on ground reaction force at a high rate.
- Significant asymmetry – something to look for in general.
Okay, now we found something. What do we do about it? We know we can cue them to increase their cadence (SEE PREVIOUS POST ALREADY), but we can also use visual or verbal feedback to try to change some loading parameters. Most of the time this is effective for pelvic drop, step width, or knee window variables. All of this plays into the R and S of RISK in the injured runner. We can reduce overall load by landing lighter and quicker. We can shift overall load by landing closer to the center of mass or with a different part of the foot. Given that these retraining tactics have only been studied in the short-term, we can only say they’re helpful short-term to attenuate load in a runner to work back from an injury. After that, it’s likely that most go back to running the way they always did anyway. That’s because it’s rarely about the way that someone runs – it’s about the training plan. The most beautifully economic runner in the world can get injured if they don’t manage their training plan appropriately. In theory, it would be helpful to help maximize running economy in the healthy runner to improve performance with gait retraining, but we don’t have a body of evidence to tell us that right now. The next post will be on the I and K of RISK, my personal favorites.
Questions? Comments? Are you a spam robot? Let me know.
Dr. Jason Tuori, PT, DPT, CSCS
References/cool running readings:
- Barton CJ. Managing RISK when treating the injured runner with running retraining, load management and exercise therapy. Phys Ther Sport. 2018; 29: 79-83.
- Souza RB. An Evidence-Based Videotaped Running Biomechanics Analysis. Phys Med Rehabil Clin N Am. 2016; 27(1): 217-36.
- Pipkin A, Kotecki K, Hetzel S, Heiderscheit B. Reliability of a Qualitative Video Analysis for Running. J Orthop Sports Phys Ther. 2016; 46(7): 556-61.
- Barton CJ, Bonanno DR, Carr J, et al. Running retraining to treat lower limb injuries: a mixed-methods study of current evidence synthesised with expert opinion. Br J Sports Med. 2016; 50(9): 513-26.
- Willy RW, Meira EP. Current concepts in biomechanical interventions for patellofemoral pain. Int J Sports Phys Ther. 2016;11(6):877-890.
No comments:
Post a Comment