This review was originally published for the American Academy of Sports Physical Therapy's (AASPT) Sports Performance Enhancement Special Interest Group research review. For more details go to https://www.aaspt.org/spe-sig
Background:
Team handball (handball) is an increasingly popular sport with nearly 19 million participants world-wide.1 The physical nature of the sport is characterized by jumping, throwing, running, changing directions, and contact.2 Due to the demands of the sport, both traumatic and non-traumatic injuries are common at all levels of play. Preventing injuries in handball would be valuable to reduce the burden associated with injury.3
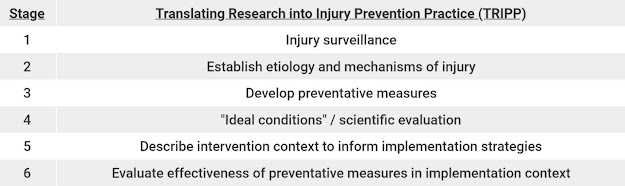
The Translating Research into Injury Prevention Practice (TRIPP) framework proposed by Finch in 2006 outlines the multi-stage process of injury prevention in sport.4
Table 1 – TRIPP framework, adapted from Finch
A complete evidence base for injury prevention begins with establishing the extent of the problem, or injury surveillance. Injury etiology and risk factors must then be identified to outline the focus of the prevention program. A program should then be tested for efficacy in a controlled setting before investigating the context of implementing the intervention in a realistic setting; this involves assessing attitudes, current behavior, and beliefs of the population of interest. Finally, the prevention program must be tested for effectiveness in-context. The purpose of this review is to highlight the current state of injury prevention research for non-traumatic shoulder injuries in handball, using the TRIPP framework as a guideline.
The definition used
for non-traumatic shoulder injuries has varied, but several studies have used
the Oslo Sports Trauma Research Center (OSTRC) Overuse Injury Questionnaire to
differentiate between “overuse” and “substantial overuse” problems.5
An overuse problem is defined as any reduced handball participation, training
volume or performance, or pain. A substantial overuse is defined as moderate or
severe reductions in training volume or in performance, or complete inability
to participate in handball. A score of > 40 on the OSTRC Overuse
Injury Questionnaire has also been used as a cutoff to indicate shoulder
injury.6,7,8
A prospective cohort study by Aasheim and colleagues investigated overuse injuries among male junior handball players throughout a handball season.3 Ten Norwegian junior handball teams (n = 145) were surveyed bi-weekly for 34 weeks on prevalence of overuse injuries during the season. The average prevalence of overuse and substantial overuse shoulder injuries was 17% and 7%, respectively, the highest of any area of the body reported. A study of 179 Norwegian elite female handball players showed a shoulder pain prevalence of 39%, with 69% of all players reporting a history of shoulder injury.9 Asker and colleagues investigated average prevalence of overuse and substantial overuse shoulder injuries in 471 Swedish junior handball players.10 Females were found to have a higher average prevalence of overuse (48%) and substantial overuse (27%) injuries than males (39% and 19%, respectively) in one season prospectively.
Etiology and risk factors:
The evidence on risk factors for overuse shoulder injuries is somewhat conflicting in handball literature, potentially because of differences in populations studied and methods of data collection. Most etiology studies have primarily investigated non-participation-related risk factors such as strength, glenohumeral ROM, and scapular control. In a prospective study on 16 female elite handball players, Edouard and colleagues found a higher relative risk of injury in players with an external rotation (ER)/internal rotation (IR) concentric strength ratio of <0.69 on their dominant arm, as measured by an isokinetic dynamometer at 45° of scaption and 240°/s.11 Interestingly, the results did not show ER weakness in the injured group, but larger increases in IR strength, thought to be adaptive for higher throwing velocities. In a cross-sectional study on glenohumeral range of motion (ROM) in 36 male and 28 female handball players, Almeida and colleagues found that those with shoulder pain had significantly greater glenohumeral IR deficit (GIRD), ER gain (ERG), and ER in their dominant arm, and less IR in their dominant arm compared to players without shoulder pain.12 The authors noted that causal inferences should not be drawn based on the study alone, as the study design did not allow for it. Clarsen and colleagues found a significant association between obvious scapular dyskinesis, lower glenohumeral total ROM in the dominant arm, and reduced ER strength (measured isometrically with a handheld dynamometer at 0° of abduction) and shoulder injury risk in 206 Norwegian elite male handball players across one season.6 Anderssen and colleagues conducted a prospective cohort study on shoulder injuries in a larger, mixed-sex cohort but failed to reproduce the findings of Clarsen et al.7 329 (168 male, 161 female) Norwegian elite handball players were followed across one season and greater glenohumeral IR ROM in the throwing shoulder was the only variable positively associated with overuse shoulder injury. The authors noted that the testing position for shoulder strength (measured isometrically with a handheld dynamometer at 90° of abduction) was different from the Clarsen study and selected for its resemblance to the handball throwing position. In a recent prospective cohort study on 344 adolescent elite handball players, Asker and colleagues found that male players with scapular dyskinesis and female players with IR or ER shoulder strength deficits (measured isometrically with a handheld dynamometer seated at 90° of abduction and 90° of ER) had increased shoulder injury rates across two seasons of play.8 Further investigations into adolescent handball players are warranted, as it seems the risk factors in this population may differ from the adult elite population.
Participation-related risk factors have not been thoroughly investigated in handball. Anderssen and colleagues did not find an association between overuse shoulder injuries and average weekly handball exposure in their prospective cohort study.7 Handball exposure was defined as the total number of minutes exposed to handball training, match play, and strength training per week (reported monthly) and did not include a measure of internal workload. Møller and colleagues prospectively studied a cohort of 679 elite youth handball players across one season to determine the relationship between changes in training load and injury rates.13 Players that increased their training load >60% in one week, relative to the weekly average of the preceding four weeks, had significantly higher shoulder injury rates than those increasing their training load by <20%. Training load was defined as the total number of hours of handball training and match play per week (reported weekly). An ER:IR strength ratio of < 0.75 (measured isometrically with a handheld dynamometer at 90° of abduction and 30 of IR) exacerbated the effect of a training load increase above 60% and between 20% and 60%. Obvious scapular dyskinesis was only an effect modifier for a training load increase between 20% and 60%. Liaghat and colleagues recently investigated the change in shoulder rotation strength through the first half of a handball season in a cohort of 292 youth elite handball players, as several studies have only taken these measurements at the start of a season.14 An increase in ER:IR strength ratio (measured isometrically with a handheld dynamometer at 90° of abduction and 30 of IR) from preseason to midseason was found with males showing a decrease in normalized IR strength and females showing an increase in normalized ER strength. Shoulder injuries were not investigated in that study.
Development of prevention programs for handball:
Exercise trials have primarily reported on either shoulder injury status or changes in risk factors following implementation of a program. Østerås and colleagues conducted a pilot randomized controlled trial on female junior handball players.15 The group investigated the effects of a shoulder exercise program on the prevalence of shoulder complaints, assessed subjectively, before and after one season of handball in 109 players. Three teams (53 players) were prescribed a three-exercise program consisting of push-ups, resisted shoulder IR, and resisted shoulder external rotation to be completed three times per week. In the intervention group, the prevalence of players with shoulder pain decreased from 34% to 11%, despite a 72% compliance rate. The control group showed an increase in shoulder pain prevalence from 23% to 36%. The trial served primarily as a proof of concept study and did have notable limitations, including size, subjective definition of injury, and methods for assessing shoulder strength (total number of push-ups pre- and post-intervention).
Anderssen and colleagues created and tested an injury prevention program in elite male and female handball players with a two-arm cluster-randomized controlled trial.16 45 male and female teams in the Norwegian Handball Federation were randomly allocated into the intervention group (22 teams, 331 players) or the control group (23 teams, 329 players) and followed for one season. The intervention, the OSTRC Shoulder Injury Prevention Programme, consisted of five exercises with different variations to be implemented three times per week during the team warm-up before training sessions.
Figure 1 – The OSTRC Shoulder Injury
Prevention Programme exercises
The program was developed by a panel of researchers, physiotherapists, and a fitness coach in the Norwegian Handball Federation, and aimed to increase glenohumeral internal rotation ROM, ER strength, scapular muscle strength, as well as improve kinetic chain and thoracic mobility. The primary outcomes investigated were the prevalence of shoulder problems and substantial shoulder problems in the dominant arm, measured in a survey six times during the seven-month season.
There were no group differences between the intervention and control other than age of males in the intervention group (1.6 years younger on average). The prevention program was completed 1.6 times per week on average, 47% less than the recommended three times per week. The average prevalence of overuse shoulder problems during the season was 17% in the intervention group and 23% in the control group. The average prevalence of substantial shoulder problems was 5% in the intervention group and 8% in the control group. The notable limitations in the study were the low compliance rate of the intervention, as well as the lack of testing the effects of the intervention on identified risk factors (strength, ROM, etc.).
Anderssen’s group followed their trial with a survey-based study assessing attitudes, beliefs, and behavior towards shoulder injury prevention.17 The aim of the study was to investigate facilitators and barriers to implementation of a shoulder injury prevention program in elite handball to inform future design. One coach (n = 44) and captain (n = 44) from each of the teams involved in the OSTRC Shoulder Injury Prevention Programme trial were surveyed about their beliefs of injury prevention and experiences with completing the program. The survey was designed based on the RE-AIM (reach, effectiveness, adoption, implementation, maintenance) framework for assessing interventions in their implementation context.18 The main facilitator to implementation for the majority of coaches and captains was the belief that the exercise program would prevent shoulder injuries. Common barriers reported were lack of player motivation and time constraints. Only 28.6% of coaches and 23.8% of players surveyed reported that they would be using the full program the next season. There were notable discrepancies amongst staff in the attitudes toward the exercise program, with the medical staff reported to be strongly positive, the coaching staff to be positive, the players to be neutral, and the administration to be unknown.
Four studies have investigated the effects of a resistance training program on changes in shoulder injury risk factors. Genevois and colleagues tested the effects of a six-week resistance training program on shoulder strength in 25 elite female adolescent handball players in a crossover study.19 Players in the first group completed two exercises (TRX suspension trainer shoulder horizontal abduction and ER at 90° abduction) with progressions twice per week for six weeks in addition to regular handball training, while players in the second group completed their regular handball training. The groups switched after six weeks, while ER and IR strength (measured isometrically with a handheld dynamometer seated at 90° of abduction) was taken before the intervention, at the six-week mark, and at the twelve-week mark. Maximal ER and IR strength improved in the exercise groups, while during regular training alone ER strength decreased and IR did not change significantly.
Mascarin and colleagues investigated the effects of a six-week resistance training program on shoulder strength in two different studies on female youth handball players with identified strength deficits. In the first trial, a two exercise program (resistance band ER at 0° and 90° abduction) with progressions three times per week for six weeks was added to the regular handball training of 13 players with ER:IR strength ratios < 0.66 (measured isokinetically at 60°/sec).20 The experimental group saw an increase in ER peak torque compared to the control group (n=12) who completed only regular handball training. The second trial repeated the study protocol but changed the exercise program to IR strengthening in 21 players with ER:IR strength ratios > 0.75 (measured isokinetically at 60°/sec).21 The experimental group did not show an increase in IR peak torque compared to the control group (n=18) who completed only regular handball training.
Fredriksen and colleagues tested the OSTRC shoulder injury prevention program in a randomized controlled trial of 57 junior handball players over 18 weeks. 22 The study aimed to identify the effects of the prevention program on shoulder ER strength and IR ROM in the intervention group (n=28) while both groups completed regular handball training. The primary outcome measurements were between-group differences in shoulder isometric ER strength and IR ROM over an 18-week period, measured both isometrically (measured with a handheld dynamometer supine at 90° of abduction) and isokinetically (Humac NORM isokinetic dynamometer at 60°/sec and 300°/sec). The intervention group implemented the OSTRC shoulder injury prevention program three times per week during regular handball warm-up. All participants filled out a weekly questionnaire documenting intervention adherence, training and match exposure, and shoulder injuries. Average dominant shoulder ER strength improved in both groups (intervention=10%, control=6%), but there was no significant group by time interaction. Average dominant shoulder IR ROM did not change in either group.
The current state of the shoulder injury prevention literature in handball is not without limitations. First, the populations studied are variable across age, competition status, and sex. Additionally, the risk factors targeted in the prevention programs have not been consistent in the literature. Many of the study designs are often “A versus A+B” in nature (where A is handball exposure and B is the intervention). This design does not allow us to determine if the effect of the intervention was specific to said intervention, or a non-specific treatment effect; without a true placebo control, we cannot be certain that the results are the specific effect of the intervention.23 Exercise dosage and adherence are also recurring issues. If the goal is to improve strength (measured in various ways across studies), exercises dosed at three sets of 8-20 repetitions, once per session without defined resistance or progression criteria are likely suboptimal. The average adherence to the programs studied are 1.6 to two times per week, lower than the recommended dosages.
Clinical Picture:
Effective injury prevention programs have the potential to be critical components of sports medicine. Decreasing the incidence of injuries in sport serves to not only improve athletic performance, but also to reduce burden on the athlete and the sports medicine team. The current state of shoulder injury prevention in handball has shown some effectiveness, yet we still don’t know the reason why it’s effective. In the junior handball population, if injury prevention programs are effective at reducing injury risk, it may not be because of rotator cuff strength or glenohumeral ROM changes. More research is warranted to establish consistent risk factors in various populations, interventions with efficacy for changing risk factors, and to refine programs to improve compliance.
References:
- Saavedra JM. Handball Research: State of the Art. J Hum Kinet.
2018;63:5-8.
- Wagner H, Finkenzeller T, Würth S, Von duvillard SP. Individual
and team performance in team-handball: a review. J Sports Sci Med.
2014;13(4):808-16.
- Aasheim C, Stavenes H, Andersson SH, Engbretsen L, Clarsen B.
Prevalence and burden of overuse injuries in elite junior handball. BMJ
Open Sport Exerc Med. 2018;4(1):e000391.
- Finch C. A new framework for research leading to sports injury
prevention. J Sci Med Sport. 2006;9(1-2):3-9.
- Clarsen B, Myklebust G, Bahr R. Development and validation of a
new method for the registration of overuse injuries in sports injury
epidemiology: the Oslo Sports Trauma Research Centre (OSTRC) overuse
injury questionnaire. Br J Sports Med. 2013;47(8):495-502.
- Clarsen B, Bahr R, Andersson SH, Munk R, Myklebust G. Reduced
glenohumeral rotation, external rotation weakness and scapular dyskinesis
are risk factors for shoulder injuries among elite male handball players:
a prospective cohort study. Br J Sports Med. 2014;48(17):1327-33.
- Andersson SH, Bahr R, Clarsen B, Myklebust G. Risk factors for
overuse shoulder injuries in a mixed-sex cohort of 329 elite handball
players: previous findings could not be confirmed. Br J Sports Med.
2018;52(18):1191-1198.
- Asker M, Waldén M, Källberg H, Holm LW, Skillgate E. Preseason
Clinical Shoulder Test Results and Shoulder Injury Rate in Adolescent
Elite Handball Players: A Prospective Study. J Orthop Sports Phys Ther.
2020;50(2):67-74.
- Myklebust G, Hasslan L, Bahr R, Steffen K. High prevalence of shoulder pain among elite Norwegian female handball players. Scand J Med Sci Sports. 2013;23(3):288-94.
- Asker M, Holm LW, Källberg H, Waldén M, Skillgate E. Female
adolescent elite handball players are more susceptible to shoulder
problems than their male counterparts. Knee Surg Sports Traumatol
Arthrosc. 2018;26(7):1892-1900.
- Edouard P, Degache F, Oullion R, Plessis JY, Gleizes-cervera S,
Calmels P. Shoulder strength imbalances as injury risk in handball. Int J
Sports Med. 2013;34(7):654-60.
- Almeida GP, Silveira PF, Rosseto NP, Barbosa G, Ejnisman B, Cohen
M. Glenohumeral range of motion in handball players with and without
throwing-related shoulder pain. J Shoulder Elbow Surg. 2013;22(5):602-7.
- Møller M, Nielsen RO, Attermann J, et al. Handball load and
shoulder injury rate: a 31week cohort study of 679 elite youth handball
players. Br J Sports Med. 2017;51(4):231-237.
- Liaghat B, Bencke J, Zebis MK, et al. Shoulder Rotation Strength
Changes From Preseason to Midseason: A Cohort Study of 292 Youth Elite
Handball Players Without Shoulder Problems. J Orthop Sports Phys Ther.
2020;50(7):381-387.
- Østerås H, Sommervold M, Skjølberg A. Effects of a strength-training
program for shoulder complaint prevention in female team handball
athletes. A pilot study. J Sports Med Phys Fitness. 2015;55(7-8):761-7.
- Andersson SH, Bahr R, Clarsen B, Myklebust G. Preventing overuse
shoulder injuries among throwing athletes: a cluster-randomised controlled
trial in 660 elite handball players. Br J Sports Med.
2017;51(14):1073-1080.
- Andersson SH, Bahr R, Olsen MJ, Myklebust G. Attitudes, beliefs,
and behavior toward shoulder injury prevention in elite handball: Fertile
ground for implementation. Scand J Med Sci Sports. 2019;29(12):1996-2009.
- Finch CF, Donaldson A. A sports setting matrix for understanding
the implementation context for community sport. Br J Sports Med.
2010;44(13):973-8.
- Genevois C, Berthier P, Guidou V, Muller F, Thiebault B, Rogowski
I. Effects of 6-week sling-based training of the external-rotator muscles
on the shoulder profile in elite female high school handball players. J
Sport Rehabil. 2014;23(4):286-295.
- Mascarin NC, de Lira CAB, Vancini RL, da Silva AC, Andrade MS. The
effects of preventive rubber band training on shoulder joint imbalance and
throwing performance in handball players: A randomized and prospective
study. J Bodyw Mov Ther. 2017;21(4):1017-1023
- Mascarin NC, De lira CAB, Vancini RL, De castro pochini A, Da
silva AC, Dos santos andrade M. Strength Training Using Elastic Bands:
Improvement of Muscle Power and Throwing Performance in Young Female
Handball Players. J Sport Rehabil. 2017;26(3):245-252.
- Fredriksen H, Cools A, Bahr R, Myklebust G. Does an effective
shoulder injury prevention program affect risk factors in handball? A
randomized controlled study. Scand J Med Sci Sports. 2020; doi:
10.1111/sms.13674
- Hartman SE. Why do ineffective treatments seem helpful? A brief
review. Chiropr Osteopat. 2009;17:10.





No comments:
Post a Comment